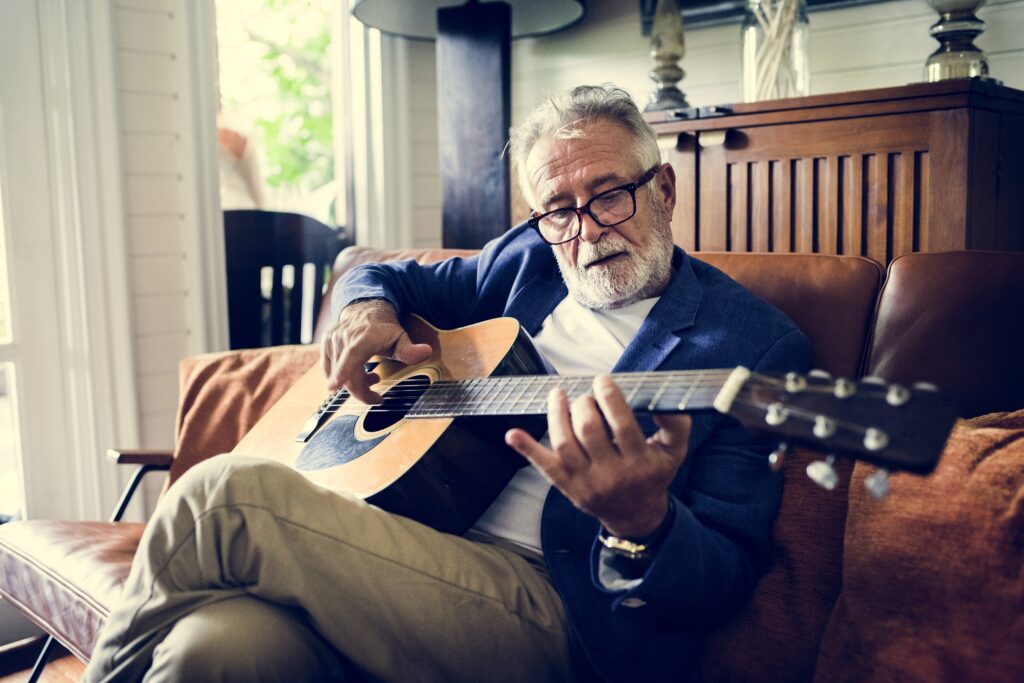
The first time Sue and Mike Miller visited their community’s senior center in Portage, MI, several years ago, they found a few people playing pool or bridge—and decided it wasn’t for them. But the couple tried again in 2022, when Portage opened its brand-new center.
The facility was impressive, but what really appealed was the expanded range of programming.
“Oh, my goodness, the things they were offering,” gushed Sue Miller.
Now the Millers, both 70, average about three days a week at Portage Zhang Senior Center, working out in the gym, taking cooking and exercise classes, enjoying lunch and volunteering. The 36,000 square foot center was built with public/private financing and designed especially to appeal to people like the Millers.
“We like to say, ‘We’re not your grandmother’s senior center,’” said Kimberly Phillips, director of senior citizen services at the center. “We are a center for active aging.”
Many senior centers around the United States are doing the same: redesigning, upgrading and evolving to meet the changing needs and interests of the newest generation of older adults. They’re trying more eclectic programming: wine tastings, coffee bars, computer courses and speed dating. They’re adding early morning and evening hours to accommodate older adults who work. Some are even dropping “senior” from their names.
There are more than 11,000 senior centers across the country, serving more than one million older Americans.
Generational differences are driving the change, according to Dianne Stone, associate director of network development and engagement at the Modernizing Senior Centers Resource Center of the National Council on Aging (NCOA). Stone recalls the center near Hartford, CT, where she began her career 25 years ago. At the time, programming consisted of a weekly meeting that opened with a flag procession and Pledge of Allegiance, followed by lunch, a speaker and an activity.
“It was like a club, and that club model was generational,” she said. “The Greatest Generation valued that collectivism. They liked potlucks and sing-alongs.”
Today, the Baby Boomers dominate the over-65 demographic, and their interests are much different. Boomers “are not joiners,” according to Susan Dillon, community programs director for the Ela Township 55+ in Lake Zurich, IL. “They’re more selective, and they cherry-pick activities.” Some may join a day trip at one center, then travel to a neighboring center the next day to play cards.
Senior centers represent one of the most widely used services among older adults in the United States. More than 11,000 centers serve more than one million older adults every day in their communities and neighborhoods, according to NCOA.
As people live longer, today’s community centers serve three different generations: the Boomers, members of the Silent Generation, who are now 79-94, as well as Generation X, the oldest of whom will turn 60 in 2025. Bridge and bingo continue to appeal to many people in their 80s and 90s, but not necessarily to those in their 60s. Senior centers must broaden their offerings to appeal to all three groups.
Stone summarizes the evolution this way: “We’ve gone from a banquet to a buffet.”
More Fitness Facilities
The biggest change: more emphasis on fitness. Boomers are more likely to sign up at older adult recreation centers with plenty of exercise options. Centers that once offered a few traditional, gentle, exercise classes, like chair yoga, are drawing new members with pickleball courts, gyms with weight equipment and cardio machines, classes like Zumba, Pilates or strength training, and evidence-based programs like Aging Mastery (NCOA’s course on aging well) and A Matter of Balance (fall prevention).
Some are also adding commercial kitchens, high-tech classrooms and comfortable spaces for reading or hanging out. They’re hiring chefs to teach cooking classes and upgrade meal programs and acquiring liquor licenses to offer beer and wine at social events.
Many senior centers, especially those in smaller communities, struggle with chronic underfunding, Stone said. But some with limited budgets are experimenting with innovative programming too. NCOA’s Modernizing Senior Centers Resource Center highlights ideas like the Repair Café in Hopkinton Senior Services in Hopkinton, MA (a daylong event in which volunteers repair household items like sewing machines, lawnmowers and furniture) or Tech Help at Calabasas Senior Center in Calabasas, CA, (a program through which local high school student volunteers provide one-on-one assistance to older adults with laptops, cell phones, smart watches and other devices). There’s also the Road to Happiness at Ela Township 55+, an eight-week class surveying the latest research on what makes people happy, adapted from a course developed by Yale University psychology professor Laurie Santos, PhD. Participants complete a survey, write letters of gratitude and discuss what they’ve learned.
Successful centers aren’t just adding more choices; they’re dumping assumptions about what older adults want, according to Dillon. She organized a bus trip a few years ago to see The Book of Mormon, a touring Broadway musical notorious for its raunchy dialogue.
Co-workers worried Dillon would get fired. The trip was a hit.
“We advertised that the show had foul language, and those who might be offended shouldn’t sign up,” said Dillon. “I don’t treat seniors with kid gloves. I never have.”
They’re also treating older adults more like adults, Phillips added. At an NCOA conference, when she shared that Portage Zhang had acquired a liquor license, shocked colleagues responded, “You let them drink?”
That kind of paternalistic attitude won’t work if senior centers want to attract new members, Phillips said.
“We need to listen to older adults, to figure out what interests them,” she said.
Phillips’ approach, along with the new center and the expanded activity calendar, has worked at Portage Zhang. Since the new center opened in 2022, membership has soared, from 1,400 to 4,000.
New Generations
When the Senior Recreation Center in Plano, TX, remodeled and reopened in 2019, its new name honored a local hero—and dropped the word “senior.” Now it’s the Sam Johnson Recreation Center for Adults 50+.
“Many Boomers are very active and don’t consider themselves ‘seniors,’” said Susie Hergenrader, PhD, assistant director of recreation for the city of Plano. “They equate the term with a sedentary lifestyle.”
The debate over the term “senior center” has simmered for decades, Stone says, but she thinks thoughtful planning and programming tailored to the community’s needs are more important.
“You could change the name to The Best Place on Earth, but if you’ve only got people sitting around watching TV, or napping in the lobby, with limited programming opportunities, you haven’t done anything,” she said.
Even with the renovation and the name change, Hergenrader said, some still think of Plano’s center as a “senior home.” First-time visitors “expect to see everyone sitting around in chairs and knitting,” she said. “But when they do come in, they’re shocked to see a recreation center with high-tech classrooms and a 3,000-square-foot fitness area.”
That’s a constant issue, Stone adds.
“The biggest challenge that senior centers face is a negative, stereotypical image as glorified bingo halls,” she said. “We also have this huge problem with ageism in this country. We view getting older as something negative, when realistically it’s something we are all doing. But there are things we can do to age well, and senior centers provide those opportunities for people.”
Expanding Technology
Like many centers, the Princeton Senior Resource Center in Princeton, NJ, shut down in the early days of the pandemic. But not for long. A team of tech-savvy staff and volunteers jumped into action, working round the clock to get the center’s programs online and to coach older adult participants one-on-one on using Zoom.
“Within two weeks, we moved all our programming online,” said Lisa Adler, MSW, the center’s chief development officer. “In addition to teaching people to get on Zoom, we helped them with online banking and apps for grocery shopping, and how to get on portals to schedule medical care.”
The center is again open to in-person programs and, in January, was renamed the Center for Modern Aging Princeton. But that “pandemic pivot” inspired an ongoing investment in hybrid technology.
Classrooms are now equipped to offer top-notch hybrid classes, with large video screens, sophisticated audio systems (including hearing loops for those with hearing loss) and 360-degree OWL cameras, which auto-track the instructor as well as student participants, allowing remote participants to easily follow along. Now, nearly 50 percent of CMAP’s 5,500-plus participants engage in the center’s programming virtually, with some joining from around the world.
“We have people coming to hybrid programs who couldn’t attend programs before when they were only in-person,” said Adler. “For example, caregivers who can’t leave the people they’re caring for can now join our caregiver support group.”
The center also continues to offer one-on-one tech help to older adults, both in person and online. Using a platform called TeamViewer, trusted volunteers can even access an older adult’s computer remotely (with their permission) to set up new software or troubleshoot problems.
Combating Social Isolation
In 2013, Illinois residents Marcia and James Dewey were poised to move to a resort community a few hours away, but a trip to Cape Cod, hosted by their local senior center, Ela Township 55+, changed their minds. They made so many new friends on the trip that they decided not to move—and became regulars at the center. They joined the Cuisine Club, took craft classes, volunteered and attended lectures, discussion groups, trivia contests, wine tastings and concerts. After James died seven years ago, Marcia joined the grief support group. Marcia, 81, uses a walker now, which she borrowed from the center’s Lending Closet. Recently, a staff member at the center helped her fix the walker and tackle an issue with her email.
“You become part of a community,” she said.
Programming may bring people into centers, Phillips said, but it’s the social connections that keep them coming back—and socializing doesn’t always need to be structured. Portage Zhang, by design, also offers quiet spaces where more introverted patrons can read or just hang out.
“We know that the impact of isolation is the same as smoking 15 cigarettes every day,” she said. “Coming to a senior center is good for your health.”
Research confirms this. “Older adults who participate in senior centers experience better psychological well-being across several measures compared to non-participants, including perceived social and health benefits, lower levels of depression, supportive friendships and lower stress levels,” according to an NCOA report.
Social isolation, of course, affects people of all ages; some centers are experimenting with intergenerational activities. In addition to its long-standing Grand Pals program (in which older volunteers read to young students in local schools), the Princeton center is experimenting with intergenerational events like nature walks and hikes. Older adults can bring their grandchildren, but anyone of any age can join.
Social connection is what keeps Donna Pollock, 93, coming to the Plano center. She recently moved into an independent living community that offers plenty of activities. But three or four days a week, she still drives to the Plano, TX, center for lunch, bingo and poker.
“My friends are here,” she said. “This place is like a second home.”
Bud Ainsworth, 81, and Jim Pruett, 71, are two of a dozen or so older adults who keep a pool game going throughout the day at the Plano center. The banter flows as players come and go.
“I enjoy the camaraderie and the fellowship,” Ainsworth said.
“We’d come on Sunday, too, if it was open,” Pruett joked.
“Senior centers aren’t just activity centers,” said Phillips. “They’re addressing a public health issue.”
Freelance writer Mary Jacobs lives in Plano, TX, and covers health and fitness, spirituality, and issues relating to older adults. She writes for the Dallas Morning News, the Senior Voice, Religion News Service and other publications; her work has been honored by the Religion Communicators Council, the Associated Church Press and the American Association of Orthopaedic Surgeons. Visit www.MaryJacobs.com for more.