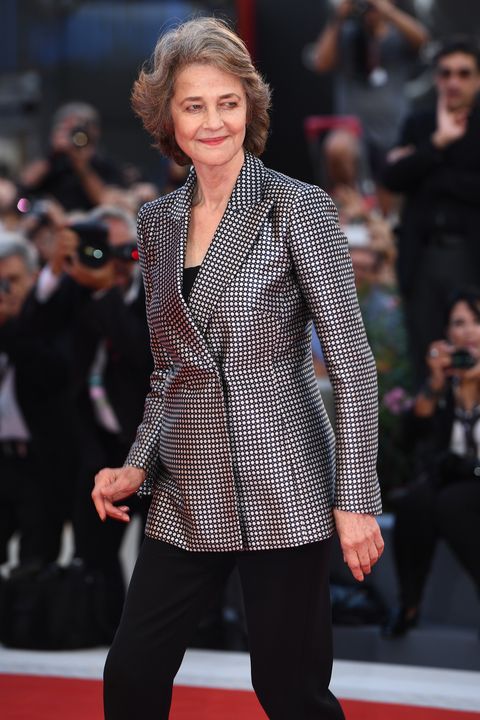
Rajiv Roy is semi-retired from venture capital, but he’s not slowing down. At age 66, he spends about half his time traveling—just in the past six months, he’s been to Colombia, China, India, Japan and Iceland—to capture birds and other wildlife through his camera lens.
Roy took up wildlife photography about eight years ago, and he’s convinced it’s helping him age more healthfully. When he’s in nature, he’s mentally engaged and physically active. He’s often out by sunrise, scanning the horizon for wildlife, tracking and observing their behavior and moving constantly to position himself for a perfect shot.
“I’ve never had a bad day outdoors,” said Roy. “It gets you away from doomscrolling or stuffing your face mindlessly as you are triggered by political news.”
A growing body of research confirms Roy’s observation: spending time in nature can help older adults stay physically active, mentally engaged, emotionally balanced, socially connected and even spiritually grounded.
Compelling evidence is piling up for the health benefits of nature. A 2019 study of nearly 20,000 participants found that those who spent at least 120 minutes per week in nature were significantly more likely to report good health and well-being compared to those with no contact with nature. The positive association was consistent across different age groups and health statuses.
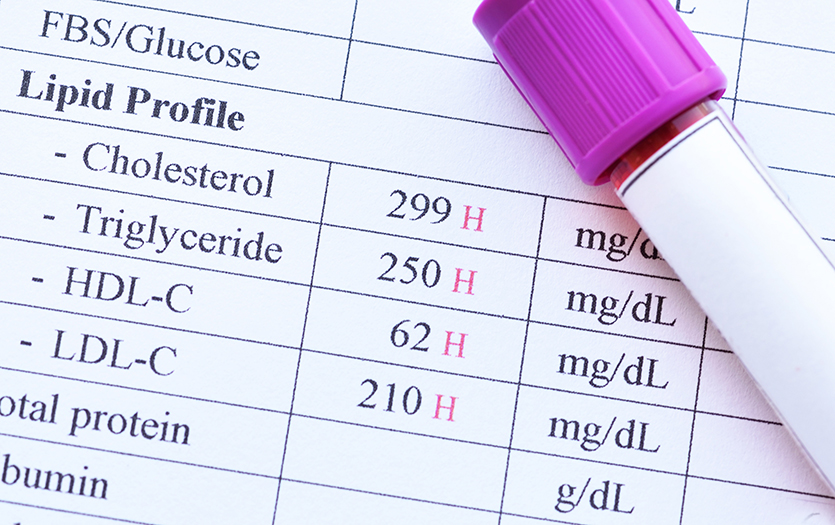
Similarly, a systematic review of studies through 2017 found that exposure to green space (such as parks or trails) was associated with wide-ranging health benefits, including reduced diastolic blood pressure, heart rate, salivary cortisol, incidence of Type 2 diabetes and stroke, and mortality. Those who live in urban areas with more green spaces are also less likely to have cardiovascular disease, obesity, diabetes, asthma hospitalization or mental distress.
The benefits are so significant that initiatives like PaRx are cropping up to encourage physicians to write “park prescriptions,” instructing patients to spend more time outdoors. PaRx, offered by the BC Parks Foundation in British Columbia, offers practical resources like quick tips and patient handouts to make prescribing time in nature easy and effective.
“Health care providers are always looking for simple, practical interventions they can make to improve their patients’ lives,” according to the PaRx website. “The beauty of PaRx is that almost anyone can increase the time they spend in nature, no matter what their physical abilities are or where they live.”
Spiritual Ground
Many cultures have long recognized the value of the natural world to human health. Scandinavians embrace friluftsliv or “open-air living,” which can range from spending days in a remote mountain hut to simply taking a lunchtime run in the forest. In Finland, saunas are a weekly or daily ritual, involving meditative sessions in heated spaces, sometimes alternated with dips in cold water or a quick roll in the snow.
In Japan, shinrin-yoku, or “forest bathing,” emerged in the 1980s as a kind of ecotherapy promoting mental and physical health. The practice involves spending time mindfully in the forest; other Asian countries, as well as Native American cultures, observe similar practices.
John Dattilo, PhD, professor emeritus in Penn State University’s recreation, park and tourism management department, was part of a team that surveyed older adult forest bathers in Taiwan. The researchers found that fostering social connections around nature-based activities could improve health and quality of life for older adults.
“Nature seems to provide a platform for connecting with other people and for cultivating a sense of meaning and purpose in life,” he said.
You hear the river running, the birds singing, and you smell the foliage or the flowers. There’s the sensation of snow or rain on your face. You don’t get that when you’re inside.
—Carol Hatch, MD
When they spend time in nature, Dattilo said, older adults often experience awe and wonder, which promotes a sense of appreciation and gratitude.
“Gratitude is such an important aspect of healthy aging,” he said. “As we cultivate a sense of gratitude, we tend to be happier and healthier and to age more meaningfully.”
Many older outdoor enthusiasts report experiencing spiritual connection and meaning outdoors.
Carol Hatch, MD, 74, a retired pediatric neurologist, finds spiritual nourishment on a hiking trail near her home in Connecticut. Now that they’re retired, she and her husband help maintain the trails as volunteers. Over the decades, she has spent many hours on the trails—sometimes alone, in reflection, and sometimes with friends, talking about what’s going on in their lives.
“It offers the possibility for introspection or for socialization, depending on how you choose to do it,” she said. “Being on the trail is a symphony of sensory delight. You can feel the sun on your skin and the wind cooling you off. You hear the river running, the birds singing, and you smell the foliage or the flowers. There’s the sensation of snow or rain on your face. You don’t get that when you’re inside.”
Nature-Deficit Disorder
In 2005, author Richard Louv coined the term “nature-deficit disorder,” identifying “the human costs of alienation from nature,” such as behavioral and physical problems affecting children who never spend time outside. Louv noted that many children born in recent decades were among the first in human history to spend all their time indoors.
Louv’s research focused on children, but many people who work with older adults observe that those who are confined indoors—whether due to isolation, mobility or health challenges—may suffer similar effects.
“Small-world syndrome” was the term that Maureen McFadden, senior services manager in Marquette, MI, and her colleagues coined for the negative effects they’ve observed among older adults who never venture outside.
“They develop a very consistent routine, they become more fearful, and they’re not exposed to new experiences or opportunities to build resilience and confidence,” she said.
Barriers to Getting Out
Since retiring about 15 years ago, outdoor activities have kept Don and Kay Wendell on the move. They chalk up about 3,000 miles a year on their bikes and spend time canoeing, skiing, snowshoeing and hiking.
“It gets your heart rate up,” said Don Wendell, 77. “And I do some of my best thinking when I’m out biking or hiking.”
But having spent his career in recreation—he was director of parks and recreation in Plano, TX, when he retired in 2009—Wendell acknowledges that many older adults don’t get out to enjoy the outdoors. He thinks that many simply don’t know where to go or how to take advantage of outdoor recreation opportunities in their area.
“I have a saying: ‘It is fun to have fun, but you have to know how,’” he said.
Other barriers that may keep older adults from venturing out, according to McFadden, include lack of transportation to safe and accessible outdoor spaces; limited physical ability or fear of falling or injury, particularly without guidance or adaptive equipment; social isolation, which can reduce motivation to try new things or venture out alone; and financial constraints, which may make equipment rentals, park entry fees or guided tours inaccessible.
To help overcome those barriers, Marquette’s Senior Center created Silver Sampler, a program to encourage people 50 and older to try a variety of outdoor recreational activities at no cost. Since 2015, Silver Sampler has offered a long list of events, including winter sports like ice skating, cross-country skiing, snow biking and snowshoeing, as well as summer activities like kayaking, stand-up paddleboarding, hiking, rowing, tour biking, trail running, mountain biking, rock climbing and disc golf.
Participants undergo an interview before joining the program. That serves two purposes, McFadden says: to assess their capabilities and to ensure their safety, but also to gently encourage participants to try new things. For example, McFadden worked with a 76-year-old woman who was hesitant to try kayaking. The woman could swim and was physically up to the challenge, so McFadden reassured her that she would stay near her and teach her paddling techniques. Not only did the woman enjoy kayaking, she came back for another kayaking trip, and with her confidence boosted, joined other Silver Sampler outings.
Silver Sampler participant Carol Steinhaus says she tried activities through the program she never would have otherwise.
“I would’ve never been on a fat-tire bike at this age,” she said. “I would not have tried downhill skiing. And I met people I would probably not have met otherwise, and I have really gained a lot from that. I’ve made lots of connections and it’s helped my life in many ways.”
Overcoming Barriers
Getting outdoors has always been a challenge for Marjorie Turner, 69. In her 30s, brain surgery left her totally paralyzed on one side of her body. She’s able to walk now, using hiking poles, but the experience inspired her to publish a series of regional trail guides for hikers with mobility challenges. She says that getting outdoors may take a little more upfront research for older adults, especially those with mobility challenges.
“It’s not always easy to gauge the accessibility of a trail before visiting,” she said. Most online sources are written for able-bodied people and often neglect to provide key information about trail surfaces or the availability of parking, benches and bathrooms. A trail rated as “easy” might be level but littered with rocks or roots, posing a fall hazard for an older person with foot drop or neuropathy.
Turner notes that rail trails—hiking trails built along former railway routes—are often a good bet for older adults. Most are fairly level, paved and handicapped-accessible. Most are located near populated areas, with access to parking and bathrooms. (Find rail trails in your state at the Rails to Trails Conservancy website.)
Turner advises older people who are venturing out into nature to never hike alone and to bring a cell phone, water and a fanny pack or light backpack. While it may take more planning to find safe, accessible places to enjoy nature, Turner says, it’s worth the effort.
“As soon as I step outside, my heart is lighter,” she said.
Transformations
McFadden says outdoor recreation can transform the lives of older adults. She witnessed that with the Silver Sampler program. One participant, Don Bode, joined shortly after retiring and moving to Marquette. He was overweight, struggled with joint pain, had been physically inactive for many years and didn’t know anyone in the area.
Bode started kayaking and hiking. He met new people and lost 60 pounds. He discovered asahi, a Finnish fitness practice, and even went to Finland to become a certified instructor. Now he teaches asahi at the Senior Center in Marquette.
Joining Silver Sampler, Bode said, made him feel part of a community and gave him a sense of purpose.
“You can wake up every morning and say to yourself, ‘What am I going to do today that’s going to keep me from aging in a poor manner?’” he said. “Or I can do something that the Silver Sampler taught me.’”

Freelance writer Mary Jacobs lives in Plano, TX, and covers health and fitness, spirituality, and issues relating to older adults. She writes for the Dallas Morning News, the Senior Voice, Religion News Service and other publications; her work has been honored by the Religion Communicators Council, the Associated Church Press and the American Association of Orthopaedic Surgeons. Visit www.MaryJacobs.com for more.