After my mother’s second broken hip, she began sleeping in her recliner in the living room. It was easier and she was small, so she slept just as well. I slept on the couch less than 10 feet away, but we argued about the temperature so much (she liked the room like a sauna) that I eventually moved into the vacant bedroom.
One very early morning, when I was helping her to her feet for one of her thrice-nightly walker-walks to the bathroom, we heard a slosh before we noticed that the carpet beneath her feet was soaking wet. It wasn’t blood or urine, it was water leaking like a loose faucet from her shins.
Water trailed her wherever she walked, and either I or her daytime aide had to follow behind her with towels, drying the path, so she wouldn’t slip. I placed large bath towels on the rug in front of her chair to sop up the excess. Where was this water coming from? She was leaking more than she drank.
Weeping edema, the visiting nurse called it. Fluid buildup in the lower extremities —thanks, gravity—that burst through Mom’s aging, dry skin as if a dam had broken.
Enter the Unna boot. The visiting nurse wrapped my mom’s calves in a sort of zinc-infused cast that works to dry out the moisture and to improve blood flow with compression. The problem with the Unna boot, however, is that it only masks the problem and doesn’t solve it. Her legs would dry out, but the nurses couldn’t put on a new boot if there was no moisture. Each time, the weeping would start again within days.
I began taking Mom for weekly visits to the wound clinic at White Plains Hospital, where they would unwrap her legs, wash them (she loved that) and then rewrap. It was difficult enough getting her to the hospital, but that became even more challenging when COVID hit. After a few visits, the hospital thought it would be safer to stop the trips and have the visiting nurses return. But while her legs were dry, the visiting nurse wouldn’t put on a new boot.
I pleaded for more preventative care—to let the legs air out for a few days and then put on a new boot before the carpet got soaked. Nope. Can’t do it if the leg isn’t “weeping.” Medicaid wouldn’t pay for a visit if there wasn’t a cause (although they had already sent a box of boots), even if that cause was only a day or two—like clockwork—from reoccurring. So one of the nurses came up with a different idea: they would put Mom on palliative care, as that would require a weekly nursing visit.
The next week, the palliative care intake nurse showed up and chatted with Mom for about a half hour. As she was leaving, she called me over to talk in the hall.
“She doesn’t have dementia,” the nurse said.
“I know,” I replied. “Who said she had dementia?”
“That’s what it says on the application.”
“Well, the application is wrong,” I said. “We’re getting palliative care so she can get weekly visits to treat her weeping edema.”
“That’s not a reason for palliative care,” the nurse said.
I explained what had been happening for the past few months and, thankfully, the nurse got it. Nurses are the best.
“I’ll change the reason on the form from ‘dementia’ to ‘malnutrition,’” she said. I thought that was going to make it sound like I wasn’t feeding Mom, but I held my tongue. It turned out to be a prescient change that I’ll write about soon.
It wouldn’t be until a few weeks before she passed that Mom’s legs would stop leaking, mostly because by then she had stopped drinking. There was not enough water left in her body.
It made me long for the puddles.
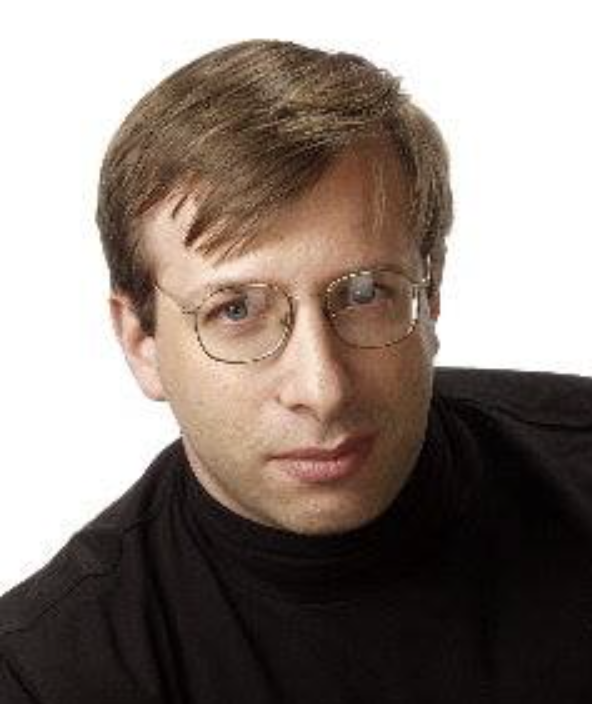
Howard Gensler is a veteran journalist who has worked at the Philadelphia Daily News, TV Guide and the Philadelphia Inquirer and has freelanced for dozens of magazines and websites. Gensler wrote the story for the 2012 movie Hysteria, starring Maggie Gyllenhaal and Hugh Dancy. In between jobs, he worked as a caregiver for his mom.



